Psoriasis is a complex chronic inflammatory skin disease, which affects about 125 million people worldwide.
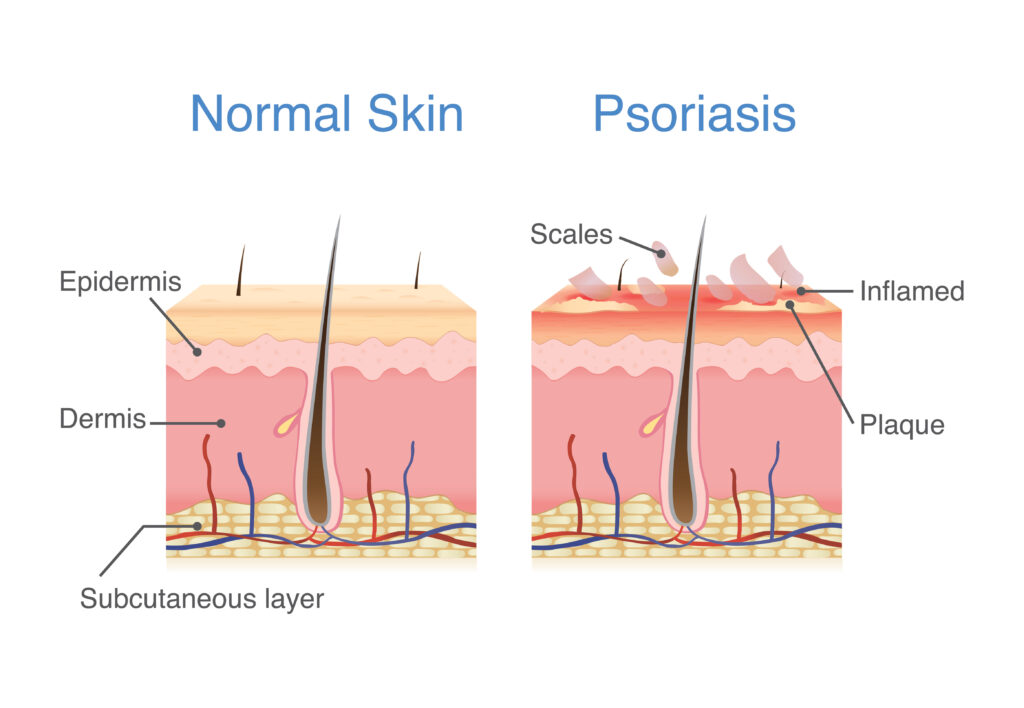
In most patients, it manifests itself with the appearance of lesions characterised by thickened skin with a silvery-white scaly appearance (plaques), often associated with itching and pain.


The areas most affected are:
- elbows
- knees
- sacral region
But the following areas may also be affected:
- genitalia
- palm of the hands
- soles of the feet
- nails
- scalp.
There are different types of psoriasis depending on the morphology of the lesions:
- Plaque psoriasis or psoriasis vulgaris: is characterised by clearly visible red plaques covered with silvery-white scales. It is the most common form of psoriasis, affecting about 90% of patients.
- Guttate psoriasis: the lesions are small (‘teardrop-shaped’), sometimes punctiform, and spread all over the skin but especially on the torso.
- Pustular psoriasis: characterised by localised pustules in various areas of the body that generally develop into scabs. There are several types, some of which are rare and serious.
- Erythrodermic psoriasis: this is the most severe form of psoriasis, but fortunately also the rarest. It involves extensive inflamed, reddened and oedematous lesions, with general impairment of the patient (fever, dehydration, oliguria, etc.).
- Inverse psoriasis: this is localised where the skin is in contact with other skin, such as the armpits, around the groin, genitals and between the buttocks, with large, smooth, red patches.
There is also arthropathic psoriasis (PsA) or psoriatic arthritis, which is characterised by the involvement of the joints and frequently derives from p. vulgaris.
The primary cause of the formation of psoriasis lesions is an autoimmune disease, which causes accelerated reproduction of skin cells that leads the skin to thicken and develop spots and plaques.
Other triggering or worsening environmental factors often include:
- Psychophysical stress.
- Mechanical trauma (such as friction, burns, scars, etc.) can cause psoriatic patches to appear in predisposed persons.
- Chronic use of certain drugs (e.g. lithium salts, tetracyclines, antimalarials, NSAIDs, …).
- Unhealthy lifestyles such as alcohol consumption and smoking, poor diet, sedentary lifestyle.
Psoriasis has a great impact on the quality of life of those affected, particularly affecting the social and relational sphere of the individual.
A study published in the Journal of American Academy of Dermatology has shown that false myths about psoriasis negatively affect patients’ psychological well-being. Research has shown that this unease is even stronger in young people.
The main complication the patient may face is the emotional impact psoriasis can cause, which can result in reduced self-esteem, anxiety and depression.
USEFUL ADVICE
To find out if you have psoriasis, it is essential to consult your doctor, who will be able to indicate the most suitable treatment.
The most common treatments for psoriasis, a chronic condition characterised by alternating switch-on and switch-off phases, are mostly for local use and therefore involve creams and lotions containing corticosteroids or keratolytic agents. Moisturising and emollient products are used as a complementary treatment and are effective during the remission and flare-up phases of psoriasis.
Given the impact that pathology can have on therapeutic adherence, even simply because of the location of the pathology, the first success is undoubtedly therapeutic compliance with treatment. This is why it is very useful to establish a direct relationship and communication with the dermatologist, to ensure that information is shared.
To keep symptoms under control, it can be important to follow some simple daily habits:
- Avoid wearing synthetic or irritating fibres and overly tight clothing
- Exposure to the open air and the sun, in the cooler hours and for a moderate amount of time, can be beneficial.
- Doing moderate exercise every day, always wearing comfortable clothing, helps both body and mind.
- Follow a healthy diet, mainly based on the consumption of anti-inflammatory foods, i.e. rich in omega-3 and polyunsaturated fats, but also vitamins, minerals and fibre.
- Clean the lesions thoroughly, using detergents and emollients approved by the dermatologist, without keeping the skin in contact with water for too long; to dry, dabbing the area with a soft sponge cloth is recommended
In the cold season, room humidification can be beneficial.
